Our COVID-19 response
31 May 2021
By the time the World Health Organisation (WHO) declared the COVID-19 pandemic in April 2020, our COVID-19 Emergency Response Group (CERG) had been established for three months. Chaired by Dr Steve Bolsin, Group Director Medical Services and Clinical Governance, this group of subject matter experts has been unwaveringly committed to providing guidance, communications and recommendations, organising additional supplies of PPE and critical care support, and prioritising the safety of our caregivers, patients, clients and communities, with our exceptional infection prevention and control processes coming to the fore.
"I remember in the early days we spent a lot of time addressing concerns around hand washing, community transmission, numbers of intensive care beds and the concept of physical distancing. We were also focused on discussing the merits and pitfalls of airborne versus droplet spread," said Steve.
"We have all learned so much in a short space of time, and have always adjusted our advice, and our behaviours, to help keep us all as safe as we could.
"As a community, Australia is so much more health literate – even with some things as seemingly basic as hand hygiene. It’s all part of our ‘new normal’."
Key to the success of the St John of God Health Care response has been the exceptional cooperation and collaboration with State and Federal Governments, and with other health care groups. This combined effort enabled us to be ready to double our ICU capacity by sourcing extra equipment, planning for repurposing units and upskilling caregivers.
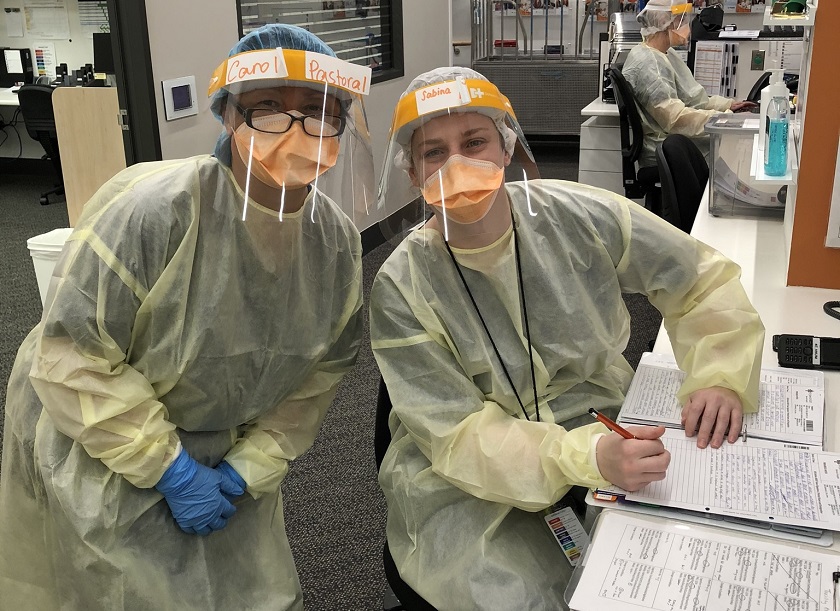
Our expert knowledge of infection control has been an integral part of the COVID-19 Emergency Response. Consistent and reliable clinical education regarding infection control was developed and delivered, with excellent outcomes for patient and caregiver safety.
As a health care provider, St John of God Health Care has had a significant role in managing this pandemic. St John of God Midland Public and Private Hospital caregivers cared for critically ill COVID-19 patients very early in the pandemic and our organisation was required to adapt swiftly to the changing landscape. Some examples of this include:
- Creating a contact tracing team to assist the Victorian Department of Health and to minimise community transmission.
- Creating the COVID-19 Command Centre to manage the second wave in Victoria.
- Ensuring patients and clients had access to celebration of the Mass televised through hospital televisions, and encouraged alternative arrangements for patients to receive the Sacrament of Anointing if approaching end of life.
- Rolling out telehealth across hospitals, community mental health services and pastoral care to reduce foot traffic while maintaining patient care plans; and offering online training and education classes for patients.
- Establishing and staffing COVID-19 testing clinics at St John of God Midland and Hawkesbury District Health Service hospitals, and offering St John of God Langmore Centre to Monash Health as a respiratory and fever clinic.
- Taking in COVID positive and suspected aged care residents to St John of God Berwick Hospital.
- Recommissioning St John of God Langmore Centre to offer the Victorian Department of Health additional beds to help manage the aged care crisis.
- Ceasing non-elective surgery in readiness for a surge in COVID-19 patients across the Australian health system.
- Facilitating work from home arrangements where it was possible.
- Upskilling caregivers and identifying additional spaces within our facilities to accommodate critical care patients, should we have been required to double our current ICU capacity.
- Procuring supply of PPE to ensure we could protect our patients, clients and caregivers from harm.
"I believe our management of the pandemic has been a success," said Dr Bolsin.
"We have kept our caregivers safe from harm, our IPC practises stood up in the face of the tests that were thrown at it, our PPE recommendations didn’t fail us, and most importantly, we have learned an awful lot – not the least that our caregivers are an incredible group of people."
Attention now turns to the vaccine program, and also to alleviating the crisis fatigue that in some cases is deep seated. Self-care is often the first thing that is sacrificed during times like these, as it often seems indulgent, but in order for caregivers to better care for others, they must care for themselves.
The incredible selflessness and generosity of caregivers across the entire organisation cannot be overstated.
"Many volunteered to step outside their areas of comfort to support those most vulnerable, to be upskilled in new areas of patient care, and to live away from their own families in order to help keep people safe. It’s been a significant team effort and one that makes us all proud."
You may be interested in
