Gastroenterologist Dr Vanoo Jayasekeran from St John of God Murdoch Hospital explains the procedure and what to expect.
What is a colonoscopy?
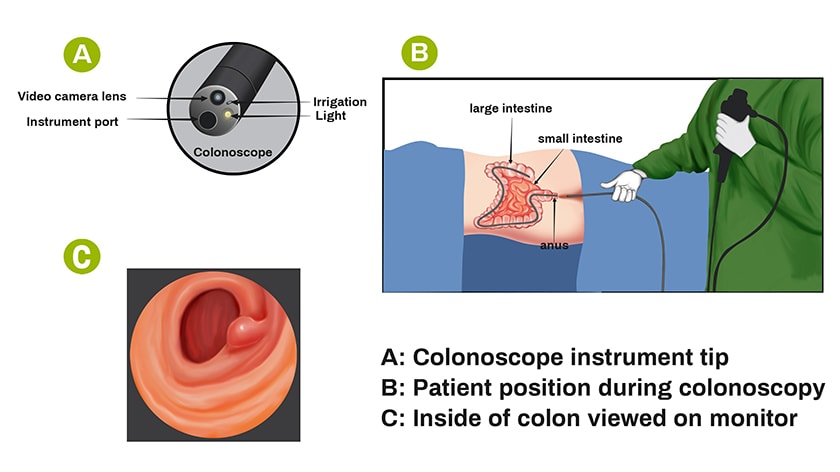
It is a direct internal examination of the large bowel. It requires a specialist doctor insert a flexible instrument through the back passage under anaesthesia. This allows high definition visualization of the inside of the colon. A certain degree of preparation is required to carry out a good quality colonoscopy. This entails several days of adjustment to one’s diet followed by drinking of bowel cleaning solution on the day before the procedure. Good compliance to these instructions allows your specialist the best chance possible in detecting any abnormalities of the bowel lining, in particular polyps and cancer.
What is the role of colonoscopy in bowel cancer detection?
Bowel cancer is the second most common cancer in Australia in both men and women. It is the cancer that also accounts for the second highest cancer related deaths in both sexes’ and the risk increases with age.
The survival rate in Australia for bowel cancer has improved significantly in the last two decades. Amongst other contributing factors; colonoscopy has played a significant role in the detection of polyps and therefore play a crucial role in early detection of colon cancer. All bowel cancer begins as a polyp, which is an abnormal growth of cells lining the inner bowel.
When should I get one?
A colonoscopy is usually requested by your General Practitioner (GP) after a medical assessment. ‘Red flag’ symptoms often signal a need for a urgent referral for colonoscopy. These include, passage of blood when opening the bowels, new changes to toileting habits (e.g. diarrhoea or constipation), recurrent need to rush to the toilet and incomplete sensation of opening the bowels.A family history of bowel cancer is also an important indication for a colonoscopy.
A personal history of previous polyps in the colon is also a strong indication for repeat colonoscopy. The interval between procedures will depend on factors such as the size, type and the number of polyps previously detected.
Another important and frequent indication for colonoscopy is when the National Bowel Cancer Screening Test returns positive. This screening test is a simple yet highly effective test in detecting cancer and large bowel polyps. It involves returning small faeces samples to a testing facility. It is a highly sensitive test designed to detect the smallest of traces of blood in the faeces. Importantly, it is designed to detect bowel cancer in people who do not yet have symptoms. It is offered every other year to all Australians between 50-74 years of age.
A low iron level or anaemia (low blood count) or indeed diarrhoea are a common indication for colonoscopy to exclude blood loss from the colon.
Who should I speak to?
You should speak to your GP or your medical specialist to discuss your health concerns. If a colonoscopy is required, a referral will be made to a specialist who has expertise in undertaking a colonoscopy.What happens during one?
You will be sedated and closely monitored. When you are comfortably sedated, you will have the colonoscope inserted through the rectum. Your specialist will examine the relevant segments of the bowel, allowing for the taking of biopsies (tissue samples for laboratory analysis) or removal of polyps.The procedure is undertaken in a hospital setting and usually takes about 30 minutes. Recovery is usually prompt and is usually carried out as a day case procedure.
What are the risks/rewards?
The major reward of a colonoscopy is the detection of polyps for the prevention of colon cancer. Other benefits include detection of all forms of colitis as causes of diarrhoea.
There are generally minimal risks associated with undertaking a colonoscopy. Bleeding as a result of removal of a polyp may occur but it is easy to manage. Bowel wall injury (perforation) is a very rare complication.








